Primer on Parkinson’s (Part 3C): Non-Motor Symptoms
The final post, Part 3C, of the non-motor symptoms series describes the impaired function of the autonomic nervous system (ANS) in Parkinson's.
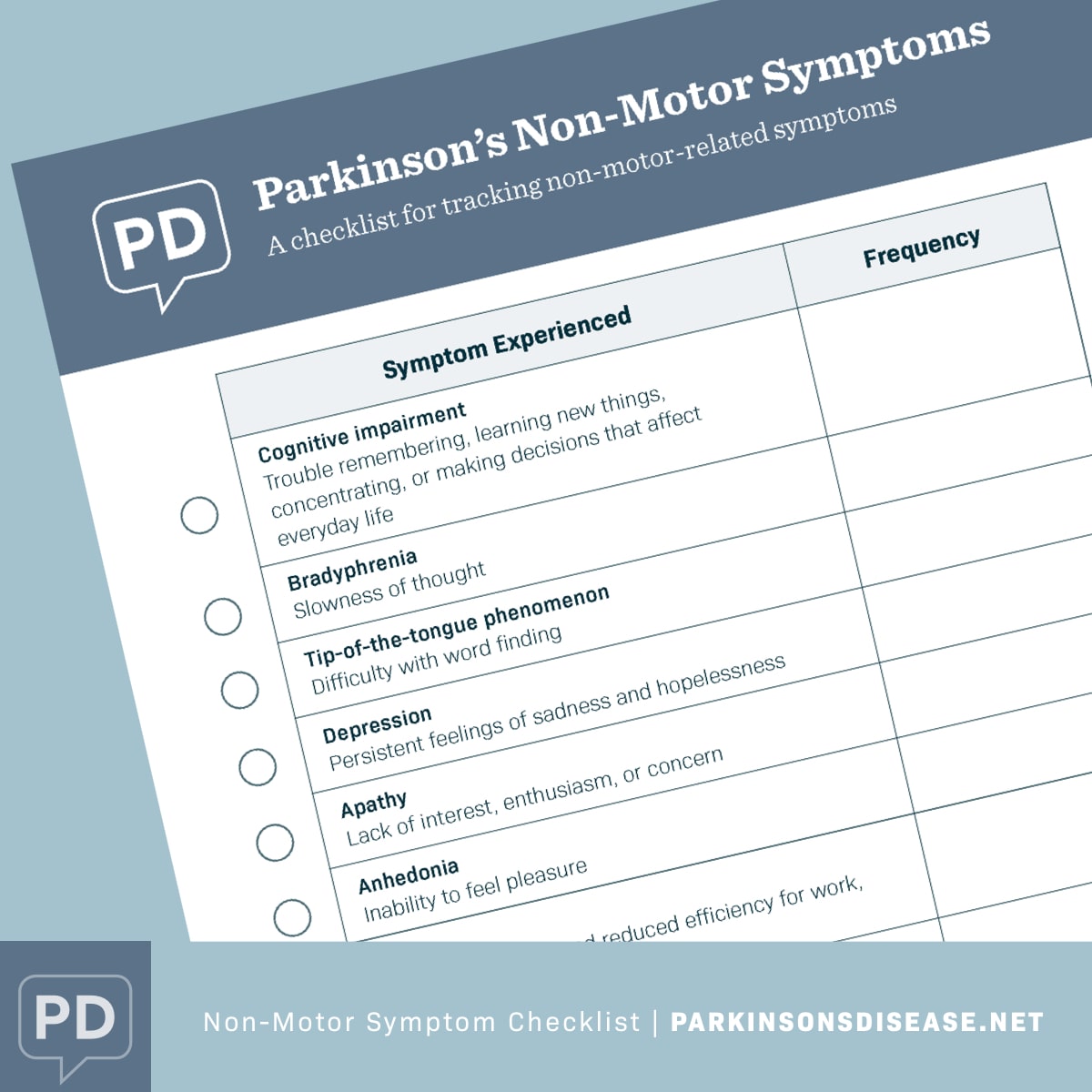
Disruption of the ANS circuitry leads to major obstacles in the quality of life in people-with-Parkinson's (PwP). The checklist of non-motor symptoms is at the bottom of the post. The importance of the nervous system to our health has been understood for many centuries. Galen, the Greek physician from the Roman Empire, noted, "Look to the nervous system as the key to maximum health."
What is the autonomic nervous system?
The autonomic nervous system (ANS) is part of the peripheral nervous system. The ANS functions unconsciously within us and it is responsible for regulating bodily functions, including the heart rate, digestion, respiratory rate, and urination. Unfortunately, ANS dysfunction is common in Parkinson's, ranging from 14 to 80 percent in occurrence.
ANS dysfunction can occur at any stage of Parkinson's. Unfortunately, ANS disturbances will directly reduce quality of life during the progression of the disorder. Thus, it is important to take measures to counter ANS-specific dysfunctions.
Orthostatic hypotension
When you are sitting or lying down and suddenly stand up, your ANS functions properly to keep the blood flowing by properly modifying blood pressure. By contrast, in Parkinson's, the ANS cannot always compensate, and the blood pressure drops when you stand up from a sitting/lying position. The PwP can become dizzy, possibly lose their balance and fall. This condition is called neurogenic orthostatic hypotension. Symptomatic orthostatic hypotension occurs in ~50% of PwP during disorder progression. Falls are always a big concern for the elderly population. Thus, you can understand the increased risk of falling in a PwP with orthostatic hypotension. The first question my neurologist asks me during my bi-annual visit is always, "Frank, have you had any falls?" To-date, and fortunately for me, my blood pressure compensates when going from a sitting to standing position.
Urinary dysfunction
Increased urgency to urinate and nocturia (a condition where you wake up from sleeping, and you need to urinate) and in general, the need to urinate more than seven times/day. This non-motor symptom of Parkinson's affects ~90% of PwP to some extent. Urinary dysfunction would negatively impact your QoL. However, there are bladder-specific exercise programs that focus on the support process.
Constipation
Due to the reduction/absence of dopamine in the brain, there is reduced muscle motion throughout the body. Reduced levels of dopamine can alter muscle contraction in the colon and produce constipation. The good news is that Parkinson's-induced constipation is treatable. Constipation can be reduced by ingesting a fiber product and staying hydrated by drinking water. And another reason to exercise is to keep the bowel muscles moving to facilitate excretion.
What's in your grocery basket?
Ten people are standing in line at the express checkout counter at the grocery store getting food for their dinner. What is in their basket? Maybe some of the same items, but likely each basket contains several items distinctive from one another.
Now imagine those ten people have Parkinson's, and their shopping basket is carrying their symptoms (motor- and non-motor). Would our basket of symptoms be the same or very different? Likely, we would have some of the same items in our basket. However, comparing the basket of symptoms of ten PwP would probably show a variety of symptoms that can be "expressed" in Parkinson's.
My shopping basket (list of motor symptoms) would include rigidity, bradykinesia, right-hand tremor, dysphagia, sialorrhoea, and micrographia. My basket of non-motor symptoms would consist of executive function (reduced ability to multi-task, takes longer to pack a suitcase and to read a map), occasionally apathetic, and night-time sleep fragmentation.
Going forward, staying hopeful, never giving up
Daily, I am doing all I can do to deal with my shopping basket of symptoms. My strategy includes taking carbidopa/levodopa, a dopamine agonist, using complementary and alternative medicine approaches, daily exercise and stretching, and being mindful. So yes, I know all about what we are up against to confront our disorder named Parkinson's.
Don't ever give up.
Don't ever give in.
Don't ever stop trying.
Don't ever sell out.
And if you find yourself succumbing to one of the above for a brief moment,
pick yourself up, brush yourself off, whisper a prayer, and start where you left off.
But never, ever, ever give up.
-Richelle E. Goodrich
Join the conversation