Melanoma Surgery and Parkinson’s
This article is the third and last of my melanoma series. In case you missed it, you can read about my diagnosis and how I've been coping in the articles:
The previous posting ended with how I've been dealing with negative thinking during the seemingly long time between melanoma diagnosis and any action.
My visit with the oncologist surgeon ended with a planned surgery of a wide excision of the melanoma site and, most likely, removal of at least the first lymph node up from my melanoma. Pretty standard plan for dealing with a melanoma that had penetrated all the way through the skin layers.
Participating in a trial
The science of melanoma treatment has been changing rapidly over the last several years. I was offered the opportunity to participate in a large trial studying various melanoma genetic markers as treatment pathway predictors and aggressiveness prediction for melanoma.
I jumped in even though my genetic marker analysis would mean pushing my surgery out about 2 weeks. Three days before the surgery, my surgeon called. Capsule bioscience gene expression profile returned.
My melanoma has a class IA recurrence profile, meaning low risk. This also estimates my risk of sentinel node positivity to be 2 percent.
Based on this risk assessment profile, the surgeon thinks it’s safe to avoid sentinel lymph node biopsy and simply perform wide excision of the melanoma. I will continue to be followed postoperatively based on the DECIDE trial protocol.
The effects of general anesthesia
More hurry up and wait. My surgery was scheduled for 7:30 AM but reporting time was 5:30 AM meaning get up at 4 AM. I had a lengthy discussion with the anesthesiologist as there are Parkinson’s implications with general anesthesia.1
People with Parkinson’s often take longer to come out from under general anesthesia, can have an exacerbation of their Parkinson’s symptoms, and a subset of people have hallucinations for a day or so.1
I was slow to awaken, my tremor was worse than normal, gargantuan headache, and I still felt a little groggy 2 days later.
The melanoma was removed
On to the important news: The pathologist reports shows clean margins on the excised sample and my melanoma is viewed as having been localized and completely removed at this time.
I’ll have to be closely monitoring going forward, meaning a dermatologist visit at least every 3 months for the future.
Checking your skin
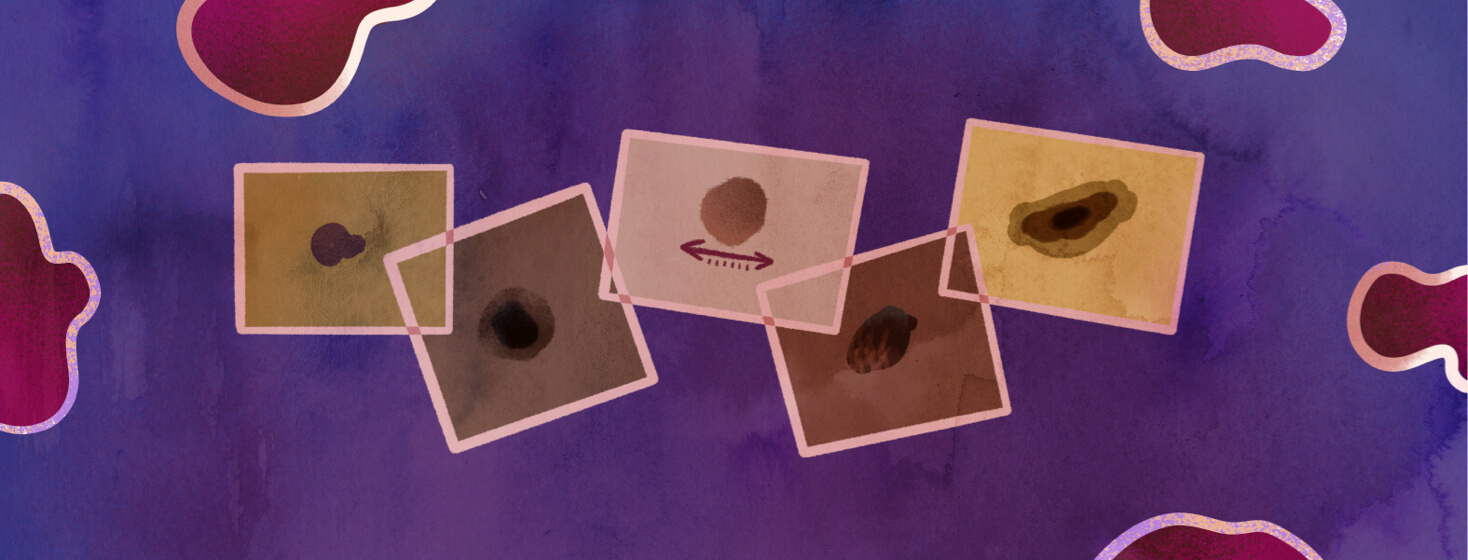
For People with Parkinson’s (and everyone else for that matter), check all over your skin at least once a month and remember the A-B-C-D-E of melanoma. If you are questioning " is it a mole or is it melanoma?" be sure to talk to your dermatologist.2
A is for Asymmetry - One half of the mole is not the same as the other.
B is for Border - Look for border irregularities. The edges of the mole are not well defined, and instead are notched, ragged or blurred.
C is for Color -Notice any color inconsistencies. The mole contains multiple colors or different shades of the same color rather than having a uniform color.
D is for diameter - Most melanomas have a diameter of at least 6 millimeters across (about the size of a pencil eraser) or more. Melanomas can be smaller than this, but most are this size or larger.
E is for Evolving - The mole changes shape, size or color.
Be sure to schedule regular visits with your dermatologist. If caught early and before it spreads, melanoma is often cured!
Join the conversation